Piles — medically called haemorrhoids — are uncomfortable, often embarrassing, and surprisingly common. If you or someone you love is worrying about blood after a bowel movement, itching, or a lump near the anus, know this first: you’re not alone, and there are safe, effective paths to help. In this blog, I explain the internal and external piles, the difference between internal and external hemorrhoids, the different stages of piles, and how Ayurveda understands and treats them — in a clear, compassionate way.
What are Piles (hemorrhoids)?
Piles are swollen vascular cushions in and around the anal canal. Normally, these cushions help with continence, but when they become enlarged or inflamed, they causesymptoms — bleeding, mucus discharge, itching, pain (especially when thrombosed), or a sense of incomplete evacuation. The clinical distinction depends on where they sit in relation to the dentate (pectinate) line.
Internal vs External—the Essential Difference
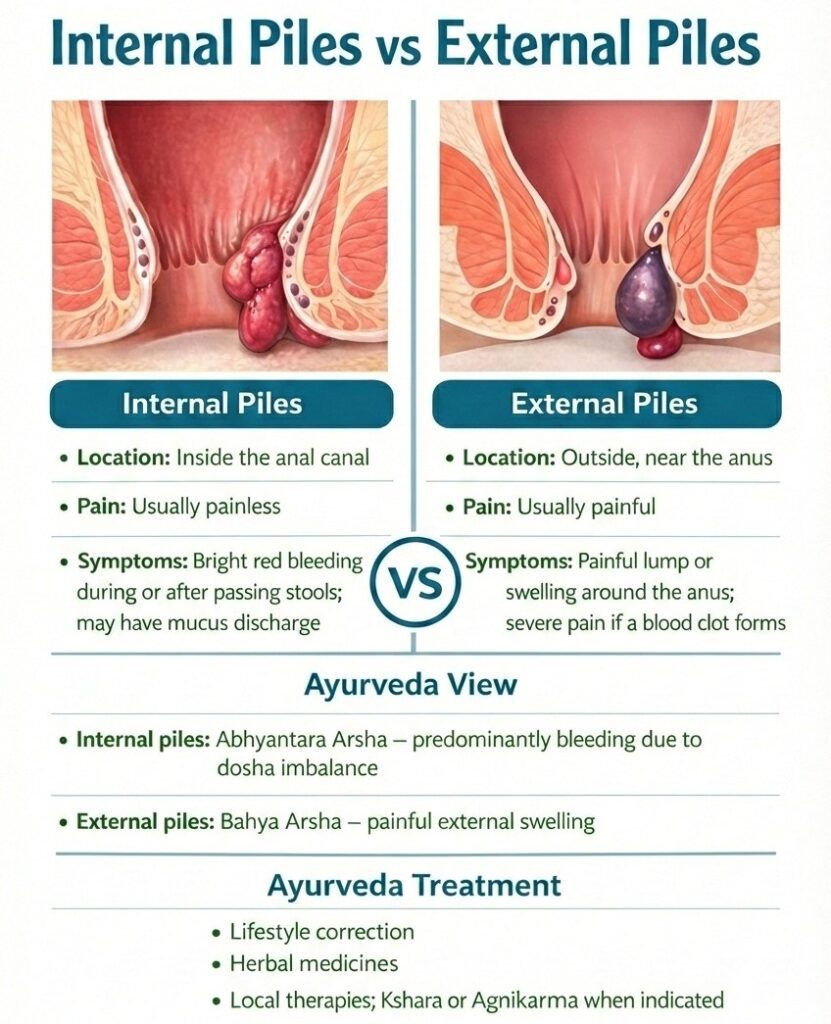
The clear way to remember the difference between internal and external hemorrhoids is location and sensation:
- Internal piles (internal hemorrhoids) originate above the dentate line and are covered by mucosa. They commonly present with painless bright-red bleeding during or after defecation and may prolapse (bulge out) on straining. Because the mucosa above the dentate line lacks pain-sensitive skin, early internal piles are often painless.
- External piles (external hemorrhoids) lie below the dentate line and are covered by skin. They are more likely to cause pain (especially when thrombosed), tenderness, and perianal swelling. External piles can form painful blood clots (thrombosis) and cause marked local discomfort.
Understanding whether a pile is internal, external, or mixed helps your clinician choose the right treatment—and it also helps you know what symptoms are expected.
The Different Stages of Piles
When people ask about the different stages of piles, they’re usually referring to how much internal hemorrhoids prolapse. The commonly used Goligher grading is practical and guides treatment choices:
- Grade I — Bleeding may occur, but there is no prolapse.
- Grade II — Prolapse on straining, but reduces spontaneously.
- Grade III — Prolapse requires manual reduction.
- Grade IV — Prolapse is irreducible, often with persistent symptoms.
Higher grades are more likely to need procedural or surgical intervention; lower grades usually respond to conservative measures and minimally invasive procedures. These classifications are endorsed in clinical reviews and international guidelines because they help match treatment to disease severity.
How Ayurveda Perceives Internal and External Piles
- Vata aggravation brings dry, hard stools, severe pain, and prolapse tendencies.
- Pitta imbalance causes bleeding, burning, and inflammation (Raktarsha).
- Kapha imbalance produces heavy, mucusy swellings and sluggish digestion.
Ayurveda Treatment for Internal and External Piles
Ayurveda care offers a spectrum from conservative self-care to para-surgical procedures. It’s useful to think in different levels:
- Conservative and lifestyle measures (first line for most Grade I–II):
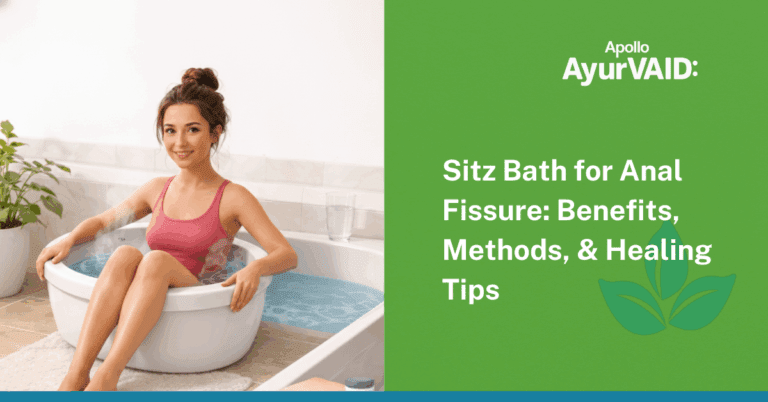
- A high-fibre diet, adequate fluids, regular walking, and the avoidance of straining are all recommended.
- Sitz baths, bowel-habit training, and specific herbal formulations (e.g., Triphala) to soften stools and reduce inflammation help most internal piles settle early.
- Targeted Ayurveda procedures (for symptomatic or recurring piles):
- Kshara Karma/Kshara Application: This is a medicated alkaline application that chemically cauterises and shrinks the pile mass; it is shown to be useful for certain low-grade internal piles.
- Agnikarma: controlled thermal cauterisation for selected, persistent lumps.
- Kshara Vasti (Matra Vasti): clinical trials reported marked improvement in many patients with bleeding piles (Grades I–III), suggesting that combined local and systemic therapy can be effective when used appropriately.
- When surgery or referral is needed:
- Fourth-degree prolapse, strangulated piles, large thrombosis not responding to conservative therapy, or uncertain bleeding patterns require referral to a colorectal surgeon or combined care. Modern guidelines recommend matching the procedure to the grade and symptoms.
| Criteria | Internal Piles | External Piles |
|---|---|---|
| Location | Inside the anal canal | Outside, near the anus |
| Pain | Usually painless | Usually painful |
| Symptoms | Bright red bleeding while passing stools | Painful lump or swelling |
| Characteristic of pain | Mostly when prolapsed or inflamed | Very painful if a blood clot forms |
| Allopathy view |
Graded (I–IV) based on prolapse; treatment depends on grade |
Not graded; treatment depends on pain and clot |
| Ayurveda view |
Abhyantara Arsha – bleeding/mucus due to dosha imbalance |
Bahya Arsha – painful external swelling |
| Basic care | Fibre, fluids, avoid straining | Pain relief, sitz bath, local care |
| Procedures |
Banding / surgery (modern) Kshara / Agnikarma (Ayurveda) |
Thrombectomy (modern) Local Kshara (Ayurveda) |