Each year, during Crohn’s disease and ulcerative colitis awareness week (Dec 1-7), I am reminded that illnesses that live inside the gut often live in silence for the rest of a person’s life. For patients and their families, the day-to-day reality encompasses more than just tests, medications, or flare-ups—it involves disrupted plans, quiet embarrassment, and fatigue that no amount of tea can alleviate. Additionally, it requires a consistent effort to know the difference between ulcerative colitis and Crohn’s disease based on their individual experiences. When someone asks for a clear Crohn’s disease definition, what they truly seek is not just medical clarity but a roadmap toward stability and hope. As an Ayurveda physician, my primary responsibility is to actively listen to patients’ symptoms, lifestyle, and the complex narrative surrounding a sudden episode. Only then can we begin crafting a personalised path that supports steady digestion (agni), reduces toxicity (ama), and enhances the overall quality of life for those navigating Crohn’s disease and ulcerative colitis.

Why this week matters
The Crohn’s disease definition is more than a line in a textbook; it is a lived biomedical and social reality. Crohn’s disease and ulcerative colitis are both inflammatory bowel diseases (IBD) but differ in their pattern and depth of inflammation. Patients often get confused between these conditions, and the answer helps in understanding prognosis, complications and management. Greater awareness helps reduce isolation, accelerates early diagnosis, and creates pressure for integrated care models where modern medicine and traditional systems like Ayurveda can work together for symptom control and rehabilitation. To know more about the difference between ulcerative colitis and Crohn’s disease, click here.
Clinical picture with an Ayurveda lens
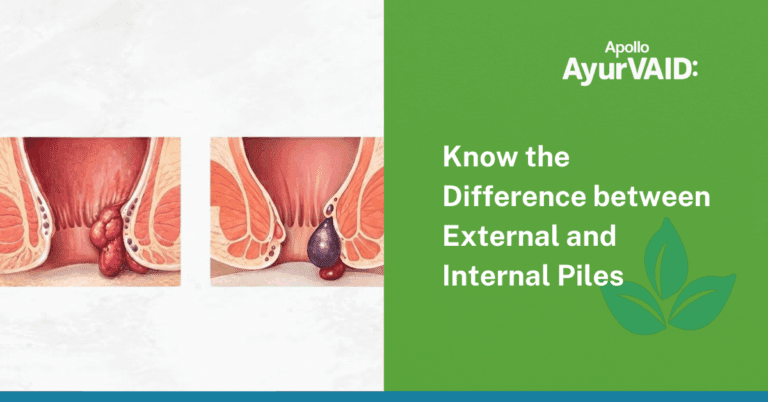
Crohn’s disease can affect any part of the gastrointestinal tract and often involves transmural inflammation (all layers of the bowel), leading to complications such as strictures, fistulae and malabsorption. Ulcerative colitis primarily involves continuous inflammation of the colon mucosa. While both ulcerative colitis and Crohn’s disease are forms of inflammatory bowel disease with overlapping symptoms, they differ significantly in the location, pattern, and depth of inflammation. These objective differences shape treatment choices and monitoring.
Ayurveda reads these patterns through the language of dosha and agni. Chronic diarrhoea, bleeding, severe abdominal discomfort and progressive weakness are seen as expressions of vitiated Pitta and Vata and of impaired digestive fire (agni) with accumulation of ama — undigested metabolic residues that perpetuate inflammation.
In Ayurveda, Crohn’s Disease (CD) is correlated with the gastrointestinal disorder known as Grahani Roga. It is also linked to conditions like Pitta Atirsra and Rakta Atisara. Ulcerative Colitis (UC) is often correlated with the advanced stage of diarrhea called Raktatisara. It is understood primarily as a Pitta-dominant Tridosha disease. Other potential correlations in classical texts include Pittatisara and Kshataja Grahani.
What an integrative treatment plan looks like
AyurVAID often uses an integrative treatment approach, when necessary, alongside pure Ayurveda practices, such as incorporating modern medical diagnostics (lab reports, scans) to identify the appropriate treatment pathway. Ayurveda therapy is explicitly designed to complement modern medical treatments. Other integrative protocols successfully combined Yoga, Naturopathy, and Ayurveda treatment when necessary.
Typical Ayurveda elements used at AyurVAID include personalised herbal formulations, digestive (deepana-pachana) measures, Panchakarma procedures (for example, Virechana and selected Vasti) during appropriate phases, and rasayana therapy to rebuild strength after an acute phase. Importantly, these therapies are planned around the patient’s current status (flare vs remission), nutritional needs, and concurrent medical treatment. The goal is pragmatic: reduce flares, avoid unnecessary surgery where possible, restore nourishment, and improve quality of life.
Practical, compassionate advice for everyday living
Gentle, easily digestible food, taken at regular intervals, and attention to meal timing supports āgni.
Avoid known dietary triggers (spicy, very high-fiber raw foods during active disease, alcohol, excessive caffeine).
Hydration, small frequent meals during flare-ups, and nutrient-dense liquids (broths, thin dals) help prevent weight loss. AyurVAID guides emphasise foods that soothe Pitta and astringent, anchoring options like cooked rice, ghee in moderation, and well-cooked vegetables.
Psychological well-being matters enormously. Anxiety, stress, and the exhausting unpredictability of IBD worsen symptoms — an observation both modern gastroenterology and Ayurveda recognise. Ayurveda’s attention to routine (dinacharya), sleep, breathwork (praṇayama), and calming therapies can reduce sympathetic overactivity and support recovery.
A note on outcomes and realistic hope
Long-term remission is an achievable and worthy goal. Integrative pathways, which combine modern diagnostics and immunotherapies with Ayurveda dietary and rehabilitative care, aim to reduce the frequency and severity of flares and to improve nourishment and function. Patient stories from integrative clinics demonstrate meaningful improvements in symptoms and quality of life when care is timely and personalised.
How to observe Crohn’s & Colitis Awareness Week meaningfully
Crohn’s and Colitis Awareness Week (observed each year in the first week of December) is an invitation: to share accurate information, to listen to those who live with IBD, to support research and compassionate services, and to reduce stigma. Small acts—a shared post about invisible illness, a supportive message to someone who’s cancelled plans because of a flare, or offering practical help—make a real difference.
If you or someone you love lives with Crohn’s or colitis, the small steady choices matter — thoughtful food, gentle activity, trusted medical monitoring, and compassionate support. Ayurveda adds value when its therapies are used thoughtfully alongside modern medicine: to rebuild digestion, reduce recurrence, and restore resilience. Awareness Week is not just a calendar event; it is a reminder that illnesses that are often invisible deserve visible care, practical support, and a world that responds without shame.