What is happening?
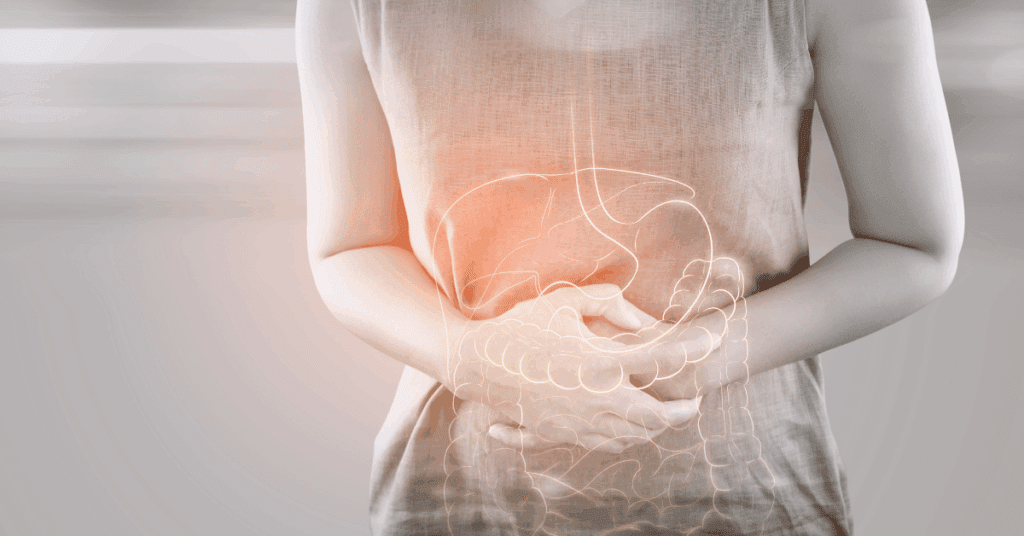
Ulcerative colitis is a long-term inflammatory disease that affects the lining of the colon and rectum. Typical symptoms are
- Frequent loose stools often mixed with blood and mucus,
- An urgent need to defecate
- Crampy lower abdominal pain
- Tiredness and sometimes fever or weight loss.
Why women can feel different
Women with UC often report more impact on quality of life, higher anxiety or depression, and flares that may be influenced by hormonal cycles, pregnancy planning or menstrual symptoms.
Emotional stress and sleep disruption can also amplify gut symptoms. Because of these gender-related differences, care that addresses both the bowel and the whole person is important.
How Ayurveda sees it
In Ayurveda, UC has features similar to Raktatisara and Grahani/Atisara — conditions where imbalanced Pitta and Vata, mucosal damage, and disrupted digestive fire (Agni) lead to bleeding, mucous discharge, pain and altered stool patterns. Treatment focuses on
(1) calming Pitta and Vata
(2) healing the intestinal lining
(3) restoring Agni (digestion)
(4) rebuilding strength and tissues (dhatu).
Ayurveda management uses internal herbal medicines, local therapies (like medicated enemas in selected cases), external soothing formulations, and, importantly, dietary adjustments tailored to the individual’s prakriti and current state.
Symptoms to watch for (female-focused)
- Persistent bloody diarrhoea or increasing frequency of stools.
- Rectal pain, tenesmus (feeling of incomplete evacuation), and urgency.
- Severe fatigue, low haemoglobin, or unintended weight loss—these signal nutritional loss and require assessment.
- New or worsening pelvic pain around menses, or mood changes tied to flares
Diet — practical Ayurveda + evidence-based recommendations
Diet is individual, but some broad, safe principles help most people:
- During flares: choose easily digestible, low-residue foods (well-cooked vegetables, steamed rice, mashed root vegetables, smoothies if tolerated) and avoid raw, crunchy, high-insoluble fibre. This is part of a workable ulcerative colitis diet plan, the best and worst foods approach.
- Avoid foods that commonly trigger symptoms for many patients: raw crucifers (like broccoli, cabbage, and cauliflower), nuts/seeds, popcorn, spicy heavy gravies, alcohol, and sugar-heavy processed foods. Because their teekshna (sharp), oily or guru (heavy) qualities can aggravate Vata and Pitta, inflame the gut lining, and obstruct digestion in ulcerative colitis. Individual triggers vary — keep a food symptom diary.
- High protein diet is recommended in ulcerative colitis — in Ayurveda, this is viewed as essential to rebuild depleted dhatu (tissues), restore agni (digestion) and recover ojas (vitality) after blood loss and wasting. We recommend gentle, easily digestible proteins (well-cooked mung dal, soft paneer, eggs, tender fish or meat broths) taken in small, frequent portions alongside digestive-supporting measures so the nourishment is absorbed, not irritating. Always customise the plan. High protein diet is recommended in ulcerative colitis during active disease to prevent muscle loss and aid in repair.
- Anti-inflammatory choices: favour nourishing, mildly snigdha (unctuous) and cooling foods that calm Pitta and soothe the mucosa — for example, gentle sources of anti-inflammatory fats (e.g., well-cooked fatty fish if tolerated, ghee in diet) and thoroughly cooked fruits and vegetables that don’t cause mucosal irritation.
- Hydration & iron: replace fluids and monitor iron — many women with UC develop iron deficiency; talk to your clinician about testing and iron treatment if needed.
Ulcerative colitis diet plan: best and worst foods
For everyday application, I suggest a simple, staged approach:
During active disease, choose soft, well-cooked grains (white rice, kanji), peeled and cooked vegetables, ripe cooked fruits, gentle protein sources (eggs, soft tofu, and dairy if tolerated), and broths—while avoiding raw fibrous vegetables, nuts/seeds, spicy fried foods, alcohol, and large amounts of insoluble fibre that commonly trigger symptoms.
As inflammation settles, gradually reintroduce fibre and variety under supervision; keep a food–symptom diary to identify personal triggers.
The combination of symptom control, nutrition (including adequate protein), stress reduction and monitoring is what helps most women live well with ulcerative colitis.
Some small studies and individual cases show that Ayurveda treatments, which use herbal remedies, medicated enemas, and herbs that help digestion, can help reduce symptoms and lower the need for steroids in certain patients.
A practical day-to-day plan
- Work with your physician to define disease activity and necessary medications — don’t stop prescribed medicines without advice.
- Consult an Ayurveda physician to design a personalised diet for ulcerative colitis patient and an ulcerative colitis diet plan best and worst foods list that suits your triggers and stage.
- Gentle Ayurveda measures (digestive teas, herbal formulations prescribed by a qualified physician, internal oleation & local therapies where indicated) can be administered.
- Monitor red flags: severe abdominal pain, heavy bleeding, high fever, fainting, very rapid weight loss — seek urgent care.