Overview
Second only to the common cold, lower back pain (LBP) is one of the most frequent medical disorders worldwide. LBP, or any pain or discomfort felt in the area beneath the 12th rib in the back and over the lower edges of the buttocks, depending on chronicity, is further classified as acute (less than 6 weeks), subacute (6–12 weeks), and chronic (more than 12 weeks).
Though anyone of any age might be impacted, instances increase between 50 and 55. Rising sedentary living, slouching posture, and stress have even younger groups experiencing LBP more and more. Among its causes, lumbar spondylosis, an age-related degenerative process of the vertebrae, intervertebral discs, and ligaments, is frequent in seniors.
Lower back pain, often known as Katishoola, Kati=Low back, Shoola= Pain, is linked in Ayurveda to a disruption of the Vata dosha and a degradation of the body’s tissues (Dhatus). Ayurveda Lower Back Pain Treatment is tailored and exact depending on the dosha involvement. With its thorough, highly individualised, protocol-driven approach (Precision Ayurveda), Apollo AyurVAID not only treats symptoms but also targets the underlying cause of the pain, therefore providing useful, specific solutions to enable you to find long-lasting relief and restore your active lifestyle.
Who Can Benefit and Who May Not: Ayurveda Treatment Scope
Who Benefits from AyurVAID’s Treatment?
Individuals undergoing:
- Lower back discomfort, either chronic or recurring
- Early to moderate spondylosis of the lumbar
- Disc bulging or hernia with reasonable neurological impact (up to grade 3)
- Pain connected to a poor posture, a lazy lifestyle, or stress
- LBP (muscle spasm, ligament strain) that is not structurally based
Who May Not Benefit from Ayurveda Treatment?
- Patients with severe spinal deformities or advanced degenerative changes that completely block the canal (grade 4)
- Patients requiring emergency surgery
- Patients with active spinal infections or malignancy
- Severely fragile or unresponsive patients
What LBP Patients Can Expect from AyurVAID’s Approach
Modern medicine classifies lower back pain as a condition of the lumbar spine, most commonly caused by muscle strain, disc herniation, spinal stenosis, or degenerative disc disease. Symptoms range from dull to stabbing pain, muscle spasms, stiffness, and restriction of movement. Risk factors include poor posture, inactivity, obesity, age-related decline, and heredity.
Traditional modes of treatment are based on symptoms and include pain medications like NSAIDs, muscle relaxants, corticosteroid injections, physiotherapy, and in advanced stages, surgeries like discectomy or spinal fusion. Chronic pain, nevertheless, makes patients habituated to drugs with adverse effects like gastrointestinal disturbances and cardiovascular issues, whereas surgery is riddled with intrinsic risks and protracted periods of recovery.
Ayurveda treatment for lower back pain is comprehensive. Patients can expect significant pain relief, reduced stiffness, improved mobility, and less inflammation and joint swelling. They can anticipate the following special advantages with Ayurveda intervention:
Relief from Chronic Pain – Panchakarma treatments such as Kati Vasti and targeted internal medicines provide deep respite from pain by removing inflammation at the root and promoting natural healing of tissues.
Less Dependency on Painkillers –Ayurveda medicines address pain and inflammation naturally, decreasing dependence on steroids, muscle relaxants, and injections. The side effects are minimal if a doctor supervises the treatments.
Enhanced Posture and Spinal Alignment – Restorative treatments help correct postural alignment through special therapies, exercises, and lifestyle modifications.
Strengthening of Supporting Muscles in the Lower Back – Ayurveda emphasises strengthening paraspinal and core muscles through rejuvenation therapies that enhance spinal support.
Stop the Degeneration of Disc and Repeated Attacks – The treatment addresses causative factors with rejuvenating therapy and lifestyle changes, which slow down degenerative processes and prevent future episodes.
Increased Mobility and Spinal Flexibility – Professional therapies enhance spine flexibility, reduce stiffness, and restore normal range of motion by lubricating joints and reducing muscle tension.
Prevent Surgical Intervention – Early treatment of root causes often allows patients to avoid or significantly delay invasive surgery.
Integrative Management – Therapies enhance overall well-being by improving digestion, sleep, and stress management, resolving comorbidities such as obesity and diabetes, and contributing to lower back pain.
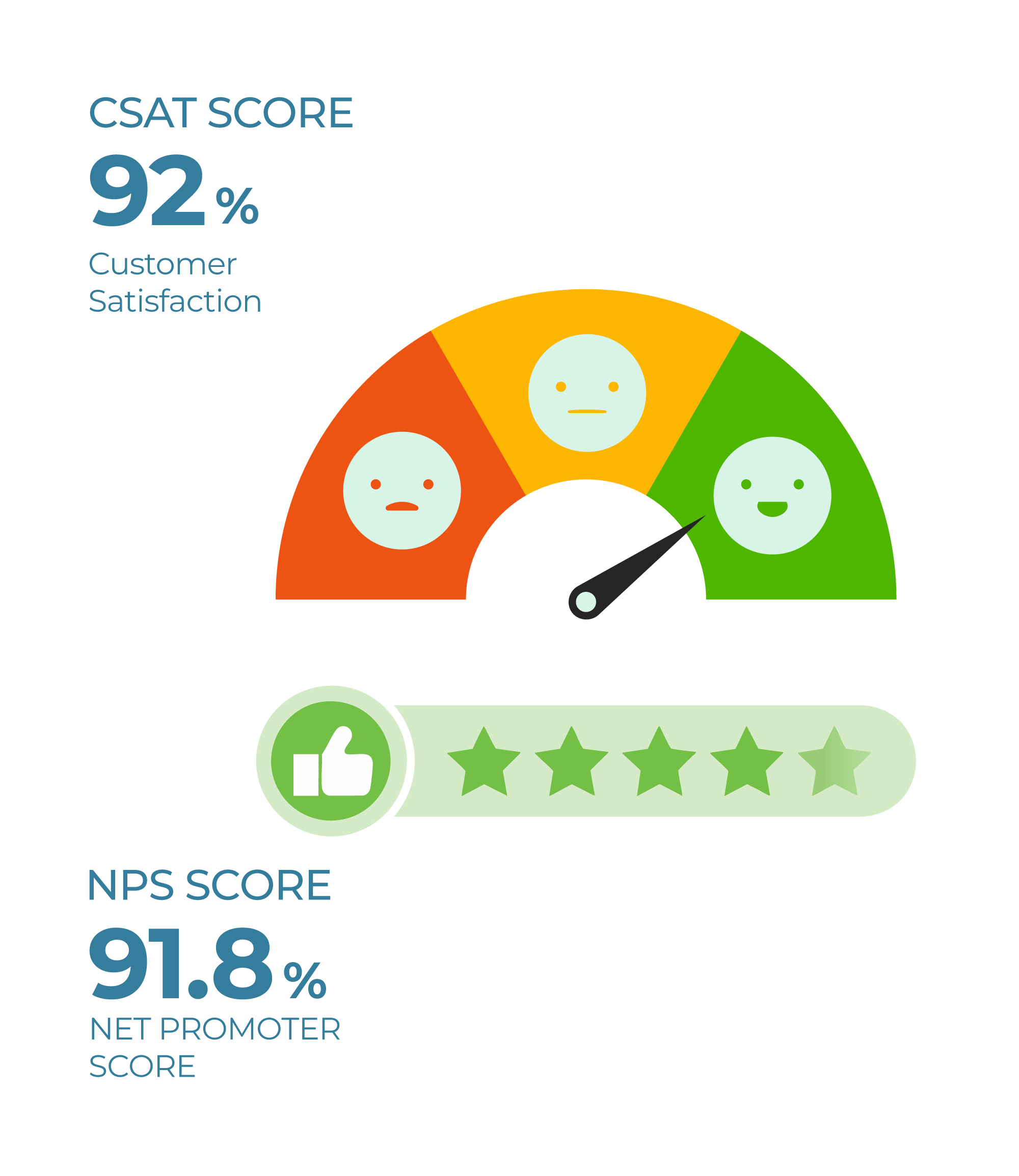
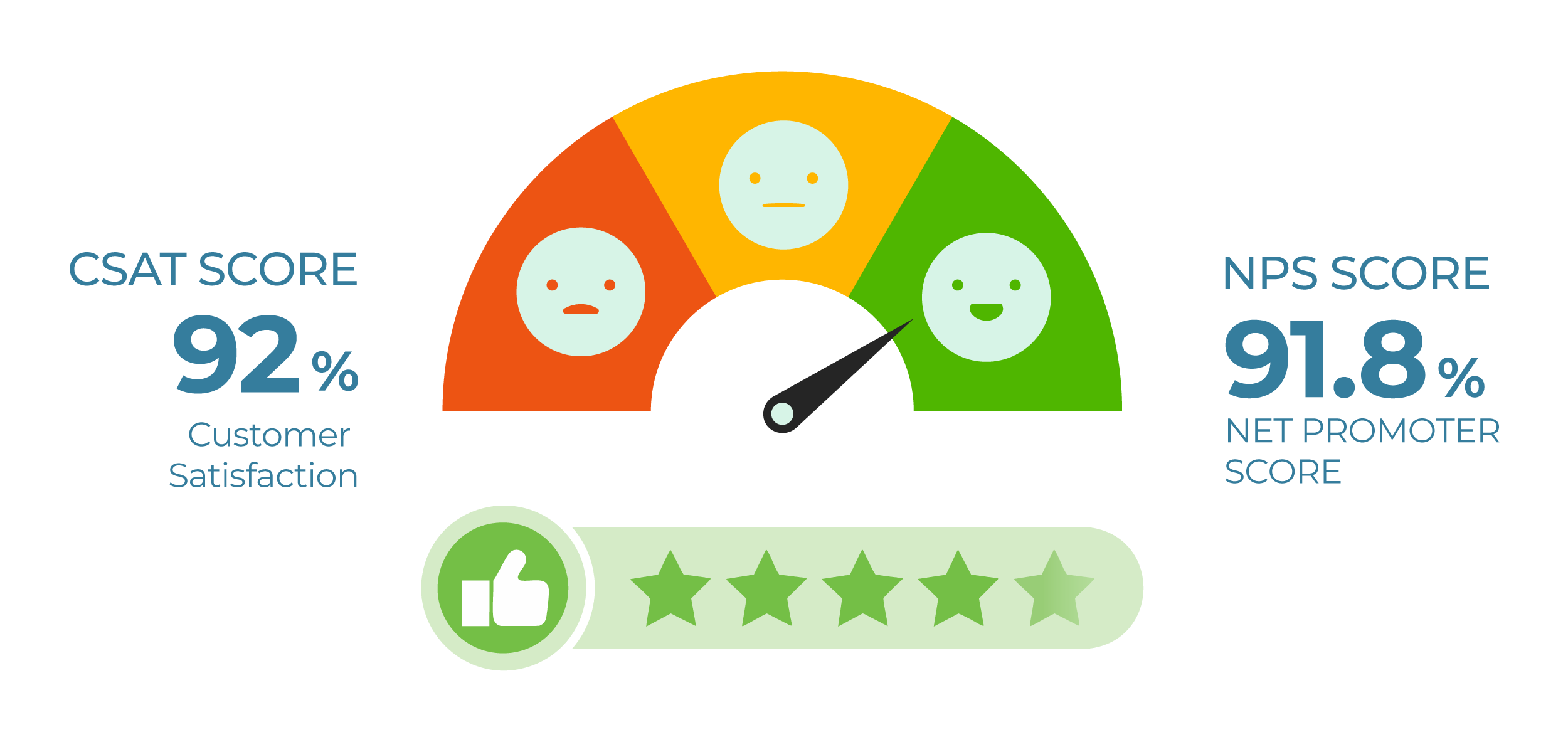
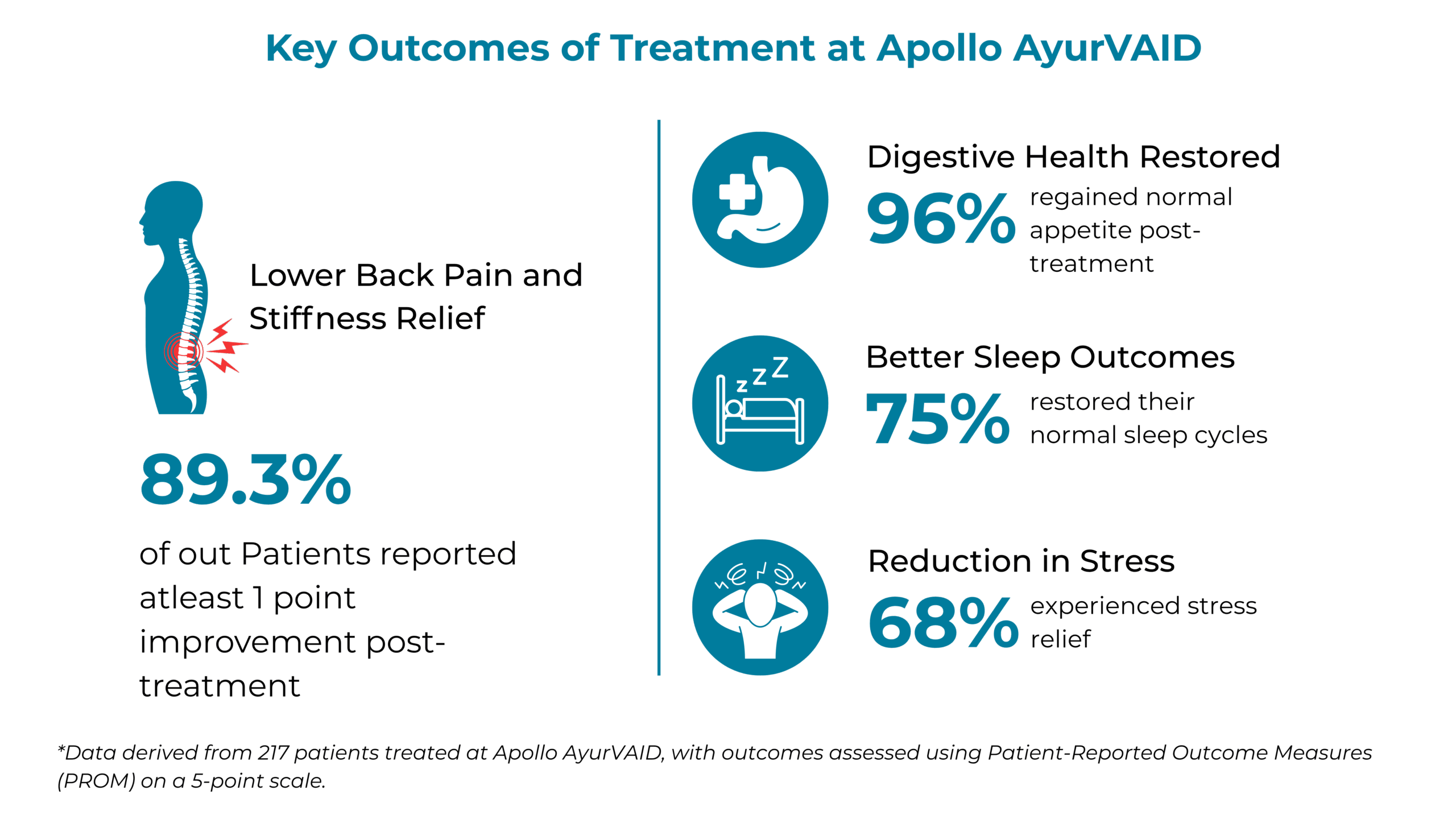
Patients highly rate our Clinical Care, Outcomes, and Service
Struggling with persistent lower back pain or stiffness?
89%* of our patients found real relief with the Precision Ayurveda Approach
*Based on PROM (Patient-reported outcome measures), rated on a 5-point scale: 1–Very Bad, 5–Excellent.
Optimising LBP Management: Ayurveda Meets Modern Medicine
| Ayurveda Terminology | Character of Pain | Modern Correlation |
|---|---|---|
| Katigraha | Localised pain associated with stiffness | Lumbar spondylosis Lumbar sprain or strain |
| Gridhrasi | Lower back pain with stiffness radiating to the lower limbs |
Lumbar canal stenosis IVDP (Intervertebral Disc Prolapse) Lumbar spondylolisthesis |
Classic pain medications like NSAIDs yield short-term benefits but are economical and widely accessible. A multi-component treatment protocol yields benefits such as fewer side effects, individualised treatment, and synergistic action of therapies.
Ayurveda addresses the root causes (Nidana) such as a sedentary lifestyle and poor posture, stops tissue degeneration (Dhatu Kshaya), and helps prevent recurrence by incorporating certain diet, lifestyle, and herbal therapies.
Causative Factors (Nidanas) for LBP
1. Uncommon causes (Direct causes)
- Causes related to the spine: Conditions like infection, tumors, IVDP, lumbar spondylosis, lumbar canal stenosis.
- Causes unrelated to the spine: Problems in other systems like the gastrointestinal tract, prolapsed uterus, osteoporosis, obesity, etc.

2. Common Causes of Lower back pain (Indirect causes)
These account for 80-90% of the cases
- Poor posture
- Injury to the spine
- Heavy physical work
- Psychosocial factors like stress, depression, or anger
- Unaccustomed lifting of weight
- Excessive travelling
- Fall or Trauma
- Smoking and drug abuse

Lower Back Pain can also disrupt Quality of Life parameters such as sleep.
*Based on PROM (Patient-reported outcome measures), rated on a 5-point scale: 1–Very Bad, 5–Excellent.
Risk Factors for LBP
- Age: Advancing age is associated with an increasing incidence of back pain.
- Weight Gain: Excess weight puts pressure on the back and can lead to lower back pain.
- Genetics: Certain reasons for back pain, including ankylosing spondylitis, a type of arthritis, are hereditary.
- Occupation: A job that involves frequent heavy lifting, pushing, or pulling can cause injury and back pain.
- Pregnancy: Lower back pain may result from pelvic changes and alterations in weight.
- Mental health: Depression and anxiety can determine how intensely a person concentrates on their pain and how seriously they think it is.
- Smoking

Signs (Lakshanas) and Symptoms (Rupa) of LBP
- Dull or sharp pain in the lower back of varied intensity
- Back spasm or muscle stiffness
- Radiating pain from the lower back to the hips or legs
- Tingling sensation, numbness, and weakness of the legs
- Pain worsening with prolonged sitting, standing, or lifting
- Painful and restricted movement
- Difficulty standing or sitting for a prolonged time
- Disturbed sleep patterns due to poor posture
- Disturbed bowel or bladder function in extreme conditions
Samprapti (Pathogenesis) of LBP
In Ayurveda, back pain (Katishoola) is primarily associated with an imbalance in Vata dosha, which governs movement, circulation, and the nervous system. When aggravated, Vata disrupts the normal functioning of the joints, muscles, and bones, leading to pain, stiffness, and reduced mobility. The pathogenesis is as follows:
Ama (metabolic toxin) Accumulation: Jatharagni Mandya (weakening of primary digestive fire) leads to the formation of Ama, a toxic, undigested residue that circulates throughout the body. Over time, this Ama weakens the Dhatwagni, the metabolic fires responsible for the nourishment of body tissues (Dhatus), particularly Mamsa (muscles), Asthi (bones), and Majja (marrow).
The accumulation of Ama obstructs the Srotas (microchannels), especially the Mamsavaha, Asthivaha, and Majjavaha srotas, leading to Srotodushti (vitiation and blockage of channels). The blockage restricts the normal nourishment of bones, bone marrow, and muscles, leading to degenerative changes in the spine, especially when coupled with Vata aggravation.
The aggravated Vata further becomes localised in the Kati Pradesha (lumbar region), resulting in clinical features such as lower back pain, stiffness, inflammation, and restricted mobility.
Dhatukshaya (The depletion of body tissues): Tissue depletion (Dhatukshaya), Vata dosha aggravation, and obstruction of channels (Margavarodha) occur. The dhatu’s include Asthi (bones), Majja (Bone marrow), and Mamsa (muscles). Degeneration is more frequent in cases of chronic lower back pain and lumbar spondylosis, where the exacerbated Vata localises in the lumbar region, resulting in pain, stiffness, and restricted movement.
Imbalance of Kapha:
Vata vitiation further disrupts the Kapha dosha balance, which governs lubrication, structure, and cohesiveness. This further causes localised stagnation, degeneration, and inflammation in the lumbar spine. The reduced lubrication between spinal joints and intervertebral discs contributes to disc degeneration and loss of shock-absorbing capacity of the spine.
In chronic cases such as lumbar spinal stenosis, Kaphavrita Vata becomes the predominant pathology where Kapha obstructs the free flow of Vata, particularly within the Majjavaha and Asthivaha Srotas. The obstructed Vata accumulates in the lumbar region, intensifying pain, reducing mobility, and producing features of nerve compression and canal narrowing, manifesting as dull, deep-seated, compressive pain, heaviness, and stiffness with neurological signs such as numbness or radiating pain.

Prevent risk-prone surgery for lower back pain and long periods of recovery
Don’t let back pain progress to surgery. Apollo AyurVAID’s treatments target the root cause with natural, personalised therapies.
AyurVAID’s 4-Step Approach to Determine Root Cause and Create Individualised Treatment Plan
1. Whole-Person Health Assessment
Conducted by our specially trained doctors, this assessment includes an in-depth evaluation of present and past complaints, Nidana Panchaka (causative factors), and disease pathways using clinical methods such as Ashta Sthana Pariksha (8-fold examination), Dasha Vidha Pariksha (10 factors), and Srota Pariksha.
A detailed history and physical exam are usually sufficient for diagnosis. However, if your pain is persistent, severe, or accompanied by other symptoms, we may recommend X-rays, MRI Scans, or other tests to rule out specific conditions.
2. Symptom Progression Tree
A comprehensive symptom progression tree, from root cause to all signs and symptoms, is derived from causative factors, imbalances in doshas, involved sub-systems, and progression.
3. Personalised Protocol-Based Care Plan
Based on the disease tree and assessments, we create an Ayurveda Lower Back Pain Treatment plan, a personalised protocol-based plan for mobility improvement, pain and inflammation reduction, and effective reversal of disease pathogenesis.
4. Disease Monitoring and Outcomes Tracking
The following standardised scales were utilised to assess treatment efficacy:
- Oswestry Disability Index (ODI): To evaluate the patient’s functional disability related to LBP.
- Visual Analogue Scale (VAS): A self-reported measure of pain intensity.
- Extended Straight Leg Raise (ESLR) Test: To assess for lumbar radiculopathy.
- Walking Distance: Ambulation distance is measured as a functional indicator of improvement.
- Aberdeen Scale: A patient-completed, disease-specific questionnaire to measure outcome in patients with lower back pain.
AyurVAID’s Protocol-Driven Treatment for LBP (Precision Ayurveda)
The Apollo AyurVAID’s protocol-driven approach (Precision Ayurveda) for Lower Back Pain focuses on controlling symptoms, preventing their progression, minimising disability, and improving the quality of life. LBP cure in Ayurveda is possible.
Ayurveda offers comprehensive treatment for LBP, which harmonises the doshas, detoxifies the system, nourishes the joints, and sustains vitality. Treatment and duration are decided depending on the intensity of the disease.
Phase 1: Anti-inflammatory & Pain Relief
This is the preparatory bodywork done to remove toxins and to balance excess doshas.
Key Goals:
- Loosen and mobilise toxins (ama)
- Alleviate localised inflammation
- Relieve pain and stiffness
Duration: Approximately 7-8 days
Treatment Protocol:
Internal Medicine:Ayurveda medicines are prescribed according to the dosha imbalance to promote digestive fire, alleviate ama, and bring relief.
Virechana (purgation) is administered after assessing the dosha’s involvement and the patient’s ability to withstand the procedure.
External Therapies: Lepa (herbal paste), Churna Pinda Sweda (medicated powder massage), and Kashaya or Dhanyamla Dhara (pouring of warm decoction), Patra Pinda Sweda (fomentation with herbal boluses), are done to reduce Ama, swelling, pain, and inflammatory response.
Phase 2: Reversing the pathogenesis: Panchakarma Therapies and Nourishing Phase
Key Goals:
- To improve the function of the affected area
- Nourish and strengthen muscles, tendons, and other supporting structures
Duration: Approximately 10-20 days
Treatment Protocol:
Abhyanga (oil therapy) and Swedana (sudation) are done as a preparatory (poorvakarma) procedure to remove toxins, balance excess doshas, and nourish and strengthen muscles and bones.
Further, Vasti (medicated enema) is administered to alleviate pain and stiffness and improve Asthi, Majja, and Mamsa Dhatu and strengthen the entire spine.
Comorbidity Management: The management of obesity and diabetes or any other comorbidities (hormonal disorders) is addressed whenever required through dietary changes in conjunction with safe therapies.
Nourishing and External Therapies: Shashtika Shali Pinda Sweda (fomentation with shashtika rice bolus), Patra Pinda Sweda (fomentation with herbal boluses), Kativasti (warm oil retention over the lower back), Kaya Seka (full-body oil pouring) are administered to strengthen the supporting structures in the lower back.
NOTE: The duration of the treatment may vary depending on the stage of the disease, severity, and comorbidities involved.
Phase 3: Maintenance
Key Goals:
- Slow reversal of symptoms
- Enhance immunity and prevent recurrence
Duration: Approximately 3-6 months
Treatment Protocol:
Rasayana Therapy: Lehyas, tailas, or grhrithas help strengthen the muscles and joints and prevent degeneration, along with external therapies such as oil massage at home.
Lifestyle Changes: Includes dietary changes, yoga, maintenance of body weight, and stress management that aid in reviving health, halting disease progression, and preventing a recurrence.
NOTE: The duration of the treatment may vary depending on the stage of the disease, severity, and comorbidities involved.
Measures to Maintain Treatment Outcomes and Prevent the Recurrence of LBP
- Nidana parivarjana (Avoiding causative factors): Excess travelling, heavy weight lifting, and bad postures, which may worsen the condition, should be avoided. A vata aggravating diet should also be avoided. Dietary recommendations focus on consuming warm, light, and easily digestible foods.
- Lifestyle modifications: Lifestyle management emphasises techniques like meditation and proper posture maintenance. Stop smoking, avoid bending while lifting, keep your spine straight, use a backrest while sitting and driving, and correct sleeping posture, which are all important.
- Lower back strengthening exercises and Yoga asanas: Flexibility and strengthening exercises, such as Lumbar/core strength and stability exercises and yoga asanas targeting the lumbar spine, are also integral components of Ayurveda treatment for lower back pain.
Ayurveda treatment for lower back pain aims for diet and lifestyle modification, along with symptom management and disease reversal.
Case Studies
Case 1: A 68-year-old male patient with acute lower back pain (Kateegraham)
Case Summary:
The patient presented with acute lower back pain, stiffness, and swelling in the lumbar region following a sprain during his morning yoga routine. He experienced difficulty in walking and restricted spinal movements, which impacted his daily activities. Clinical examination revealed marked tenderness and muscle spasm over the lumbosacral spine with limited flexion (20°) and extension (5°). Pain severity was rated 5 on the VAS scale.
He underwent a 5-day Ayurveda treatment involving Choorna Pinda Swedana with medicated powders and oils, and internal medications.
By discharge, the patient reported significant relief: pain reduced from 5/10 to 1/10, spinal flexion improved from 20° to 40°, and extension improved from 5° to 15°. Walking difficulty decreased from moderate to low, sleep quality improved from fair to good, overall wellbeing increased from 2/5 to 4/5, and stress levels reduced from 3/5 to 1/5. The Aberdeen Low Back Pain Scale improved from 63% to 25%.
No medications were required post-discharge. Dietary guidelines, lifestyle modifications, and a follow-up review after two weeks were advised.
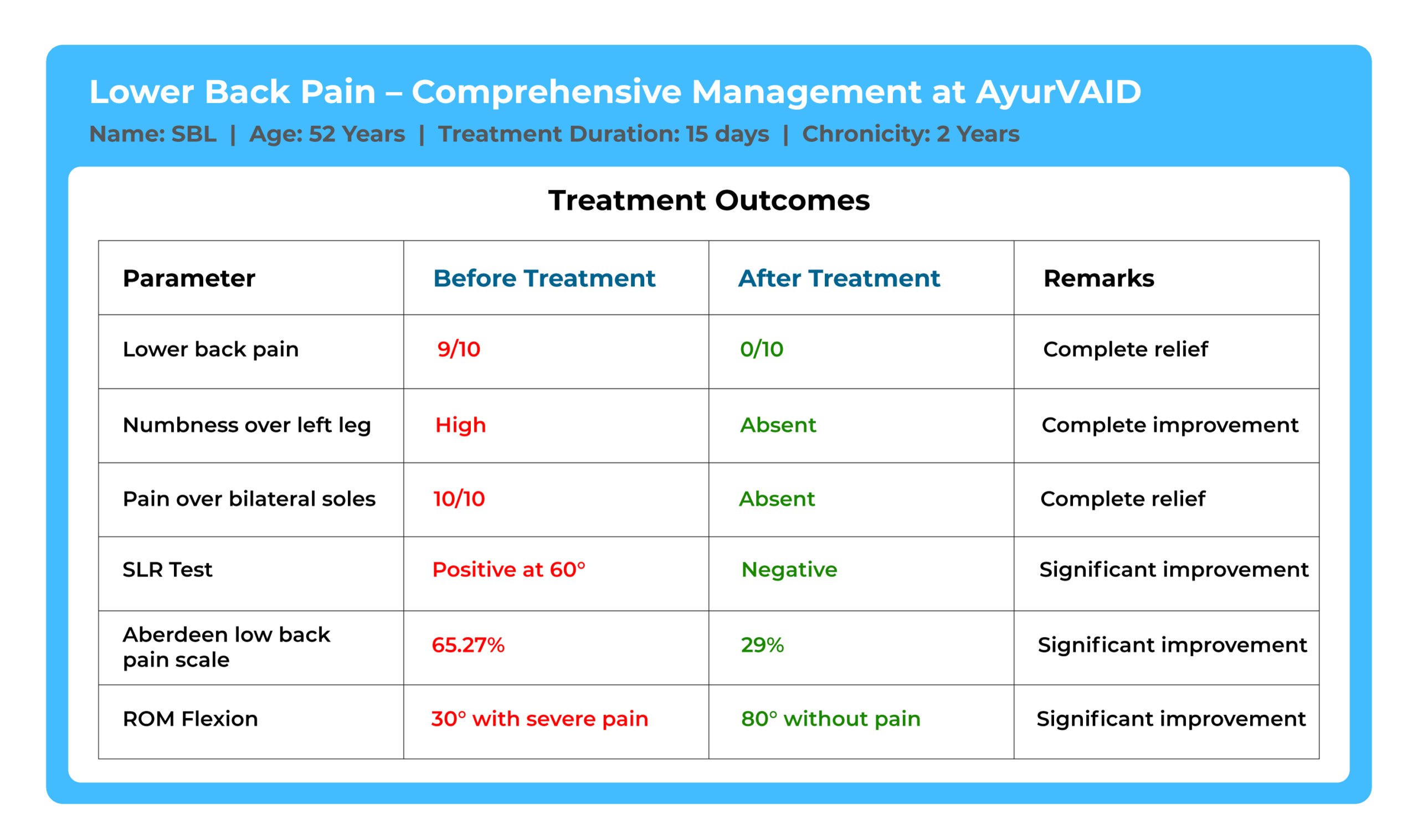
Case 2: A 52-year-old male with chronic lower back pain and lower limb discomfort
Case Summary:
The patient presented with chronic lower back pain for 2 years, worsened by prolonged sitting, along with numbness in the left leg, severe bilateral sole pain, and walking difficulty. Clinical examination revealed tenderness, restricted spinal mobility, and reduced range of motion. Pain was rated 9/10 on the VAS scale, and the Aberdeen Low Back Pain Scale score was 65.27% at baseline.
He underwent an 18-day Ayurveda treatment including Sarvanga Abhyanga, Patra Pinda Sweda, Virechana, Kayaseka (Pizhichil), Taila Basti, and Kashaya Basti, along with internal medications.
Post-treatment, pain reduced from 9/10 to 0/10, spinal flexion improved from 30° (with severe pain) to 80° (without pain), and extension improved from 10° to 20°. Lateral bending increased from 5° to 30°, numbness reduced from high to absent, and walking difficulty improved from high to absent. The Aberdeen score improved from 65.27% to 29%, and patient-reported outcomes showed a shift from "Poor" to "Excellent" in all parameters.
Discharge advice included a light, warm diet, avoidance of exertion, daily oil massage, and a follow-up after one month.
Scientific Publications
- An ayurvedic approach to a case of low back pain (katigraha) with special reference to lumbar spondylosis; 2021, Research article: This case study documented the treatment of a 44-year-old male patient with lumbar spondylosis using classical Ayurvedic therapies like Abhyanga, Swedana, Kati Basti, and Basti. Over 8 days of treatment, the patient demonstrated a significant reduction in low back pain (80% improvement in VAS score), stiffness (66% improvement in range of motion), and disability (76% improvement in Oswestry Disability Index). X-ray findings showed partial recovery of lumbar lordosis. The patient tolerated the therapy well. This study highlights the potential role of Ayurvedic therapies in managing degenerative spine conditions.
- Successful Management of Severe Low Back Pain with Ayurveda in Lumbar Spondylosis: A Case Report; 2024, Case study: A 59-year-old man with an 8-year history of lumbar spondylosis presented with severe low back pain, bilateral leg discomfort, and functional disability. Diagnosed as Katigraha under Ayurveda principles, he underwent a 9-day treatment plan including three consecutive Niruha Basti and one Anuvasan Basti, along with supportive Ayurveda medications. Marked improvement was observed: lumbar pain reduced from 8 to 2 (VAS), leg pain from 7 to 1, and ODI score from 49 to 18. Flexion and extension ranges improved measurably highlighting the potential of Ayurveda interventions in managing chronic lumbar spondylosis, particularly in mild to moderate stages.
- Ayurvedic management of recurrent lumbar pain, disability, and leg pain after posterior decompression with transforaminal lumbar interbody fusion in prolapsed intervertebral disc: A case report; 2025, Case study: A 46-year-old woman with persistent lower back pain showed notable improvements in pain (VAS reduced from 7 to 2), mobility, and daily function after undergoing Ayurveda rehabilitation. Therapy included abhyanga, kati basti, and yoga-based physiotherapy. Objective improvements were observed in grip strength and Oswestry Disability Index (reduced from 58 to 22). The case highlights how a structured Ayurveda protocol may support recovery by addressing both structural and functional imbalances.
Hear from our patients!
"I experienced severe low back pain after working with a heavy CNC machine, and after an MRI confirmed a back problem, my friend recommended AyurVAID Hospitals. After a 7-day Ayurvedic treatment at AyurVAID, my pain has reduced by 90%, and I can now walk without any problems, feeling much better."
Mr. PN, 24 years
“I came all the way from Seattle to AyurVAID Hospitals after finding them on Google, and during my 14‑day stay, I was cared for by a truly professional, dedicated team in a clean and beautiful setting. Thanks to their holistic approach—including excellent food, personalized therapies, and attentive caregivers—I experienced a dramatic improvement in my lower back pain and would highly recommend their world‑class, natural treatments.”
Mr. RK, 38 years
Frequently Asked Questions (FAQs)
References
Did the information meet your needs?
As we work hard to improve our services, your feedback is important to us. Please take a moment to help us serve you better.
Disclaimer
The information provided in this blog is for general informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician, Ayurvedic practitioner, or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment.
Stay Connected to Health and Wellness
Subscribe to our hospital newsletter for the latest health tips, updates on services, patient stories, and community events. Sign up today and stay informed!
Listen to our patient’s voice
Ayurveda Doctors for Lower Back Pain





Dr. Bheema Bhatta