- AyurVAID Pharmacy
Polycystic Ovarian Syndrome (PCOS) is one of the most common hormonal and metabolic disorders that occurs in women of reproductive age. In Ayurveda, this condition is equivalent to Pushpaghni Jataharini. The Sanskrit word Pushpaghni means destroyer of ovum, and Jataharini is a state where fertility and birth are hindered.
Ayurveda attributes PCOS to an imbalance of the menstrual cycle, metabolism, and overall reproductive health. Insulin resistance is a common condition associated with women who have PCOS. This imbalance may disrupt the normal functioning of the ovaries, resulting in a range of symptoms that are noticeable throughout the body.
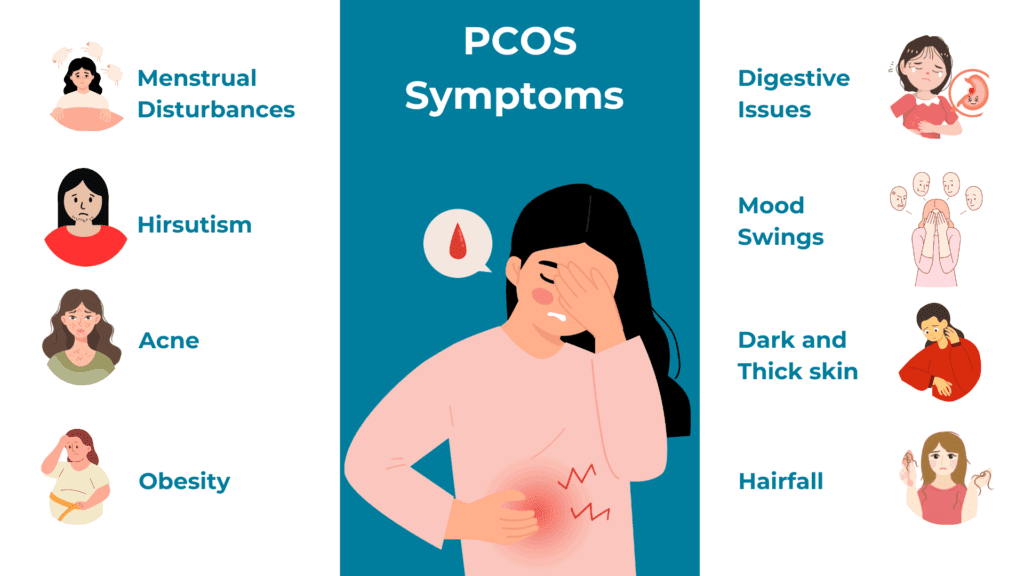
Some of the common symptoms are irregular or no periods, weight gain or inability to lose weight, acne, excessive facial and body hair, thinning of hair, mood swings, including anxiety and depression, and problems with fertility.
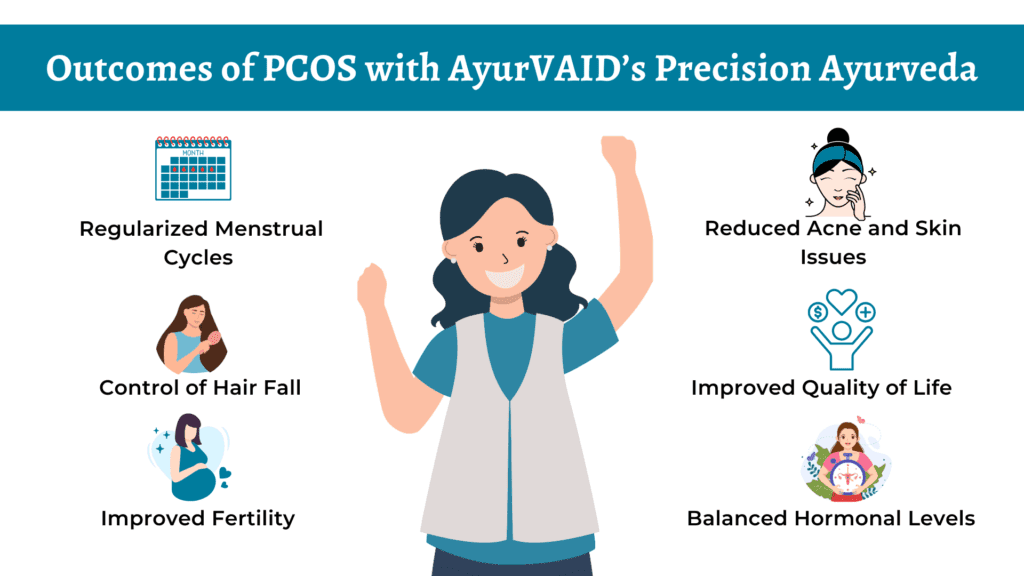
Apollo AyurVAID employs an integrated, individualised, and protocol-driven approach (Precision Ayurveda), addressing the root causes of PCOS rather than treating only its symptoms. An expert team of Ayurveda physicians conducts a comprehensive whole-person health assessment to design a personalised protocol, comprising classical Ayurveda medications and therapies, as well as individualised diet and lifestyle modifications.
At Apollo AyurVAID, Ayurveda treatment for PCOS focuses on preventing further progression of the disorder, restoring hormonal balance in the woman, and, ultimately, assisting the woman to establish a healthy menstrual cycle and fertility to improve her quality of life.
A Precision Ayurveda approach can assist individuals with PCOS at different stages – newly diagnosed people or those on long-term hormonal medication, individuals looking for support for fertility issues or metabolic imbalance, etc. Apollo AyurVAID’s approaches are especially relevant for the following patients:
1. Women with Irregular Periods and Hormonal Imbalances
If you have heavy, scanty or infrequent periods, Ayurveda can help get your cycles back on track naturally by restoring hormonal balance through individualised treatment plans and dietary changes.
2. People dealing with Skin, Hair, or Appearance-related Issues
Ayurveda has gentle, side-effect-free treatments that can help improve individual skin clarity and hormonal health for women with acne or dark skin patches on their body, like acanthosis nigricans.
3. People dealing with Weight and Metabolic Issues
If you are dealing with early-stage diabetes, insulin resistance, and/or abdominal obesity, Ayurveda detox, herbs, and dietary recommendations can be used to help promote fat metabolism and improve insulin sensitivity.
4. Patients Looking to Avoid or Transition from Hormonal Pills
Ayurveda offers safer, more comprehensive treatments that aim to address the underlying imbalance, regardless of whether you’ve recently been diagnosed or are worried about long-term use of synthetic hormones.
5. Women Seeking Assistance with Fertility and General Health
If you’re trying to conceive or want a more comprehensive approach to mood, energy, sleep, and reproductive health, Ayurveda’s whole-person care can help restore harmony and vitality.
Ayurveda aims to reverse the underlying causes of PCOS, but in some cases, it might not be appropriate or adequate on its own:

Modern medicine views polycystic ovarian syndrome (PCOS) as a chronic metabolic and reproductive disorder. PCOS is charecterised by enlarged ovaries with numerous cysts, absent or irregular periods, insulin resistance, increased androgen levels (male hormone), and a long-term risk for type 2 diabetes, cardiovascular disease, or endometrial hyperplasia.
Conventional treatment options for PCOS consist of hormonal contraceptives to manage symptoms, insulin-sensitising drugs such as metformin, cosmetic treatments for acne and hirsutism, and fertility medications. These treatments may relieve symptoms in the short term, but they usually do not treat the underlying cause of the Polycystic Ovary Syndrome (PCOS) and may have unintended side effects such as changes in mood, changes in weight or dependence on medicines.
Ayurveda treatment for PCOS takes a comprehensive, long-term, and cause-based approach.
At Apollo AyurVAID, PCOS management focuses on:
According to the principles of Ayurveda, Polycystic Ovarian Syndrome (PCOS) is the result of a combination of genetic, lifestyle, diet and psychological factors. The following outlines the most common factors associated with PCOS:
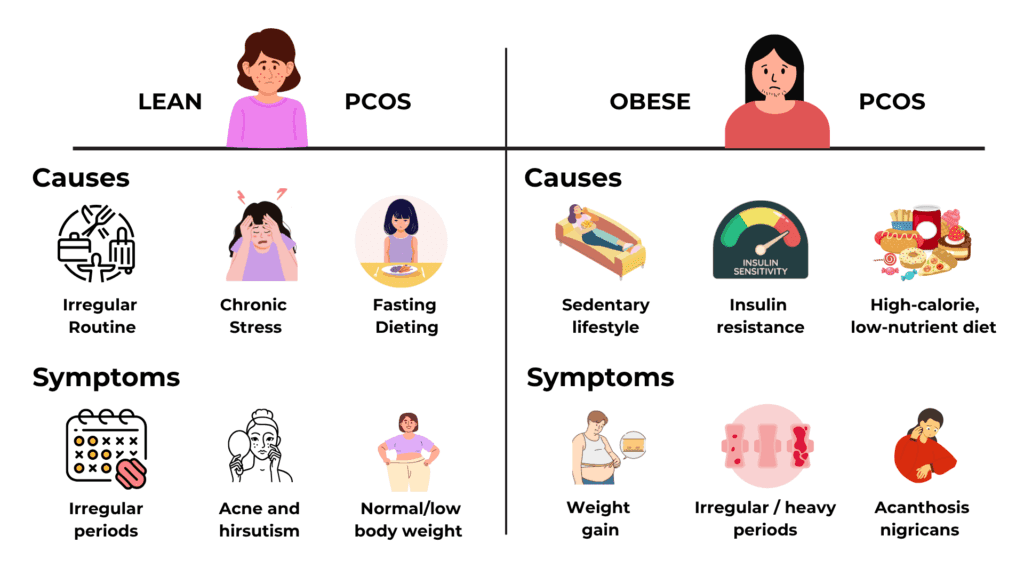
PCOS varies for lean and obese individuals. Lean PCOS is due to hormonal dysregulation resulting from stress, while obese PCOS is due to metabolic disturbance.
Lean PCOS
Obese PCOS
Ayurveda addresses both types – by restoring digestive health and balancing hormones through a combination of internal medicines, dietary adjustments, lifestyle modifications, and Panchakarma therapies. By reducing stress, Ayurveda adopts a holistic approach that extends beyond symptom management to enhance overall health and well-being significantly.

The symptoms of PCOS, or polycystic ovarian syndrome, can range from mild to severe. These include:
| PCOS Severity | Description | Typical Presentation |
|---|---|---|
| Mild | Symptoms are minor and often go unnoticed by the individual | Daily life is largely unaffected. Occasional irregular periods or mild skin/hair changes |
| Moderate | Symptoms become more visible and may require treatment, but are still manageable | Irregular periods, mild to moderate acne, some excess hair, and mild weight gain |
| Severe | Pronounced symptoms, significantly impacting quality of life and fertility | Very irregular/absent periods, significant weight gain, severe acne, pronounced hair growth or male-pattern baldness, and trouble conceiving |
Although PCOS isn’t specifically mentioned in Ayurveda, it is described as various conditions having similar symptoms:
AyurVAID employs a structured, protocol-driven approach to ensure effective treatment and sustainable recovery for patients with Polycystic Ovarian Syndrome (PCOS).
1. Whole-Person Health Assessment
Conducted by our specially trained doctors, this assessment includes an in-depth evaluation of present and past symptoms, Nidana Panchaka (causative factors), and hormonal imbalance pathways using comprehensive clinical methods such as Ashta Sthana Pariksha (8-fold examination), Dasha Vidha Pariksha (10 factors), and Artava Vaha Srota Pariksha (reproductive channel examination). Relevant laboratory tests, including hormonal profiles (LH, FSH, and AMH), and imaging (transvaginal ultrasound for ovarian morphology), are integrated for a thorough evaluation.
2. Disease Tree
We map your condition from root causes to symptoms by identifying specific dosha imbalances, agni disruption, and channel blockages. This reveals how hormonal irregularities progress to create metabolic changes, menstrual disruptions, skin issues, and fertility challenges, providing a clear pathway for targeted intervention.
3. Personalised Protocol-Based Care
Your individualised treatment plan combines classical Ayurveda medicines, Panchakarma procedures, and lifestyle modifications that address diet, exercise, and stress management. We focus on restoring hormonal balance, regulating cycles, and reversing metabolic disturbances.
4. Monitoring and Outcomes
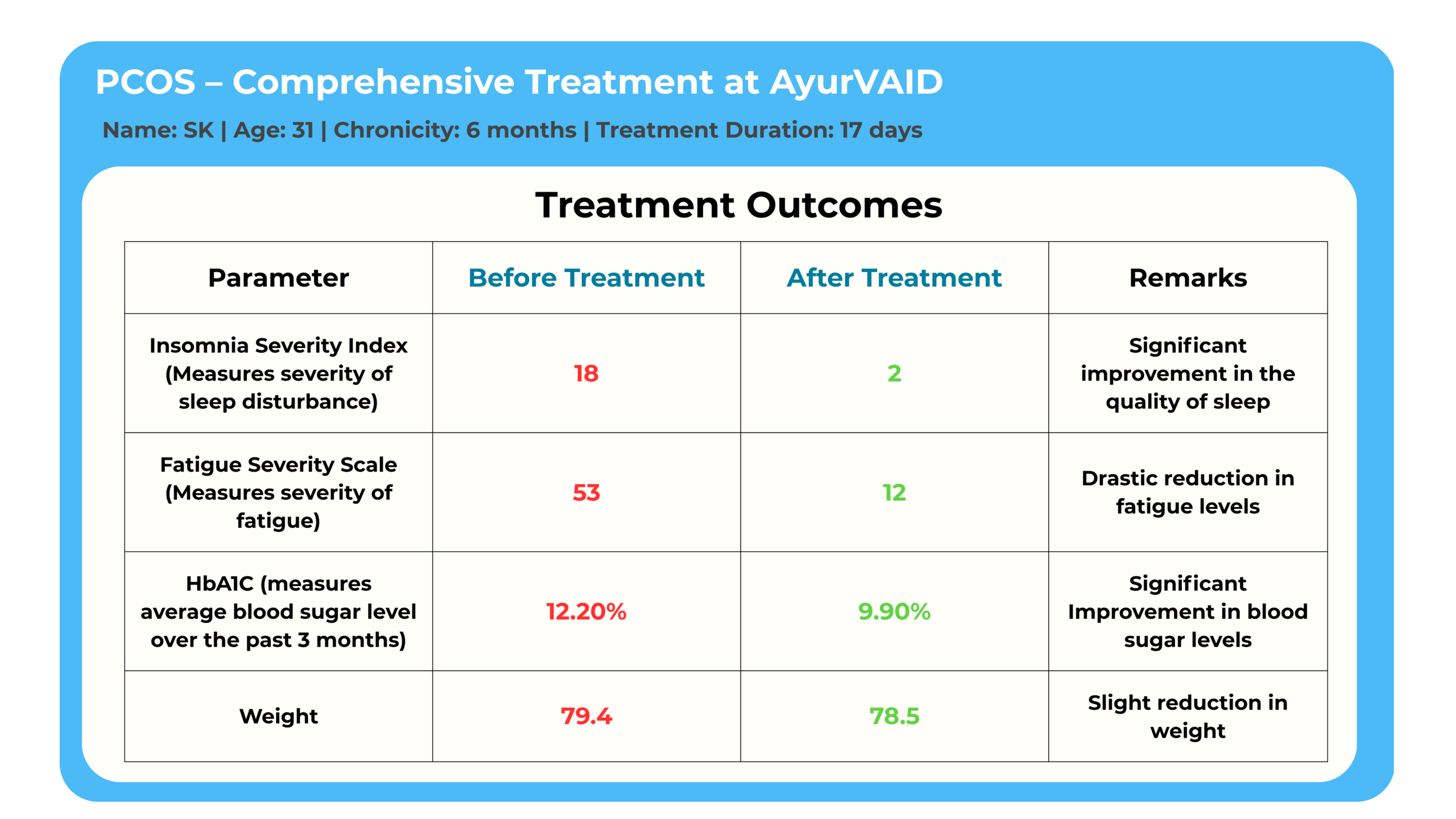
We track progress using established measures, including menstrual cycle regularity, ovulation induction, and key metabolic parameters, to ensure comprehensive improvement and long-term health restoration.
AyurVAID adopts a scientifically grounded, protocol-driven approach to managing PCOS through Precision Ayurveda, with Panchakarma as a core treatment modality. This holistic strategy targets the root causes of PCOS and promotes long-term health outcomes.
AyurVAID’s Ayurveda Treatment for PCOS incorporates the following principles:
Additional considerations include:
The Panchakarma therapy begins with Poorvakarma, a preparatory stage designed to loosen toxins, balance the doshas, and enhance the digestive fire (Agni). This stage addresses acute symptoms, including metabolic toxins (Ama), inflammation, and hormonal imbalances.
Duration: Approximately 14-15 days of intensive therapy
Internal Medications: Customised formulations to balance doshas, boost Agni, aid digestion, hormonal alignment, and expel Ama for immediate relief
External Therapies:
Administered based on the condition of the patient
In Ayurveda, Rasayana therapies are designed to nourish and rejuvenate the body, thereby enhancing overall health and well-being. The medications have shown promising results in regulating hormonal imbalances, promoting endocrine health, and improving ovarian function.
By combining Rasayana with lifestyle modifications, Ayurveda Treatment for PCOS provides a sustainable approach to managing the onset and progression, while enhancing overall health and fertility outcomes.
Note: These steps are done under the surveillance of doctors on an IP basis. The duration of treatment may vary depending on the severity of the hormonal imbalance, the extent of metabolic disturbance, the presence of associated symptoms (such as acne, hair loss, or weight gain), and any coexisting conditions, including thyroid disorders or insulin resistance.

AyurVAID follows a structured, protocol-driven approach to ensure effective treatment and sustainable recovery.
To ensure effective treatment and track progress, baseline values are taken using:
"I was suffering from persistent skin rashes, severe itching, PCOD, hormonal imbalance, weight gain, and irregular periods. Despite being on allopathic medication, I found no lasting relief. That’s when I turned to Ayurveda and underwent a 21-day treatment at Apollo AyurVAID. The experience was transformative—my symptoms reduced significantly, and I now feel energetic, rejuvenated, and deeply relieved."
Mrs. R, 34 years"
As we work hard to improve our services, your feedback is important to us. Please take a moment to help us serve you better.
The information provided in this blog is for general informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician, Ayurvedic practitioner, or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment.
Subscribe to our hospital newsletter for the latest health tips, updates on services, patient stories, and community events. Sign up today and stay informed!







Popular Searches: DiseasesTreatmentsDoctorsHospitalsWhole person careRefer a patientInsurance