- AyurVAID Pharmacy
An anal fissure is a small tear in the lining of the anal canal, which can cause severe pain and bleeding, most often when passing stools or immediately afterwards. In Ayurveda, anal fissure is known as Parikartika (“Pari” = around; “Kartika” = cutting pain), which describes the piercing, cutting pain that one experiences during this condition. Anal fissures can affect people of any age group and are very common among those with anorectal disorders.

Anal fissure treatment at AyurVAID goes beyond just pain relief and targets the underlying causes of the problem to restore anorectal health for the long term. The goal is to heal the tear, prevent it from recurring, and also to develop healthy bowel habits using evidence-based Ayurveda treatment protocols. Patients with fissures experience the following specific benefits:

According to Ayurveda, Parikartika, or fissure, is primarily caused by the derangement of Vata dosha, associated derangements of Pitta dosha, and affects the twak (skin), rakta (blood), mamsa (muscle), and Purishavaha srotas (excretory channels). The most common contributory factors include:
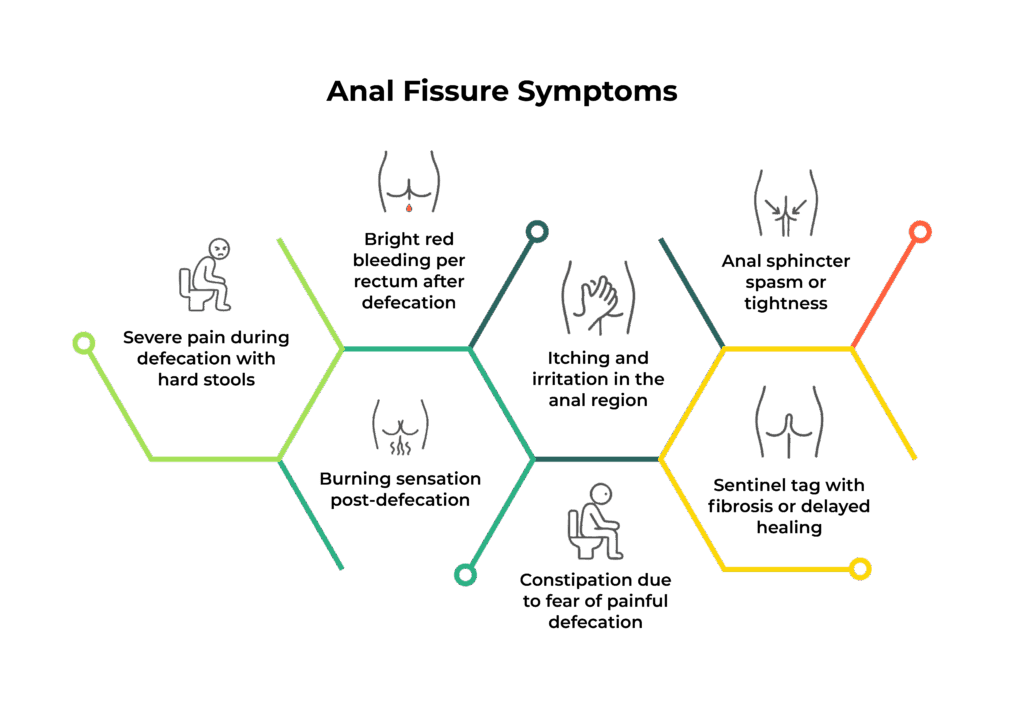
Parikartika is described as a condition that causes intense cutting-type pain in the anal region. The condition can present acutely or become chronic, with symptoms worsening if left untreated. These include:

AyurVAID employs a structured, protocol-driven approach to ensure effective treatment and sustainable recovery for patients with Fissure-in-Ano.

Apollo AyurVAID employs a precision Ayurveda approach to manage Anal fissures by addressing the root cause and effectively managing local symptom manifestations, such as pain, spasm, and bleeding.
1. Pain/Inflammation Reduction:
Objective: To relieve acute pain, sphincter spasm, soothe inflammation, and prepare the tissue for healing.
Local Therapies:
2. Promoting Healing:
Objective: To balance doshas internally, enhance digestion, heal mucosal lining, and regenerate local tissues
Internal Therapies:
3. Diet and Lifestyle Modifications:
Objective: To prevent recurrence by supporting digestion, gut motility, and tissue regeneration
Dietary Plan:
Lifestyle Guidance:
4. Maintenance Phase (Outpatient-Based)
Objective: Long-term tissue support, recurrence prevention, and gut regulation
Note: Treatment duration and specific therapy selection are tailored based on the chronicity, comorbidities (e.g., IBS, IBD, pregnancy), and severity of the fissure.

AyurVAID follows a structured, protocol-driven approach to ensure effective treatment and sustainable recovery in Anal Fissure. To ensure effective treatment and track progress, baseline values are taken using:
Condition: Fissure-in-Ano
Chronicity: 6 months (Pain episodes for 1 month)
Gender: Male
Treatment Duration: 7 days (26/02/2024 to 03/03/2024)

Case 1: A 23-year-old male with chronic Fissure-in-Ano and rectal bleeding
Case Summary:
The patient presented with severe pain and burning sensation during defecation, accompanied by bleeding per rectum and progressive weight loss over a period of one year. The symptoms had been persistent for the past 7–8 months and were significantly affecting his quality of life.
Based on clinical examination, a diagnosis of chronic fissure-in-ano was made. The patient underwent a 12-day Ayurveda treatment protocol consisting of internal medications along with localized therapeutic procedures such as Sthanika Abhyanga, Nadi Sweda, and Thaila Poorana.
Following completion of the treatment, the patient experienced complete relief from pain and rectal bleeding. Bowel movements became regular and painless, appetite and sleep improved, and overall vitality and well-being were restored.
Case 2: A 35-year-old female with chronic Fissure-in-Ano and sentinel tag
Case Summary:
The patient presented with complaints of pain and burning sensation around the anal verge for a duration of six months, along with a visible mass per anum. The symptoms were aggravated during defecation and menstrual cycles. Clinical examination revealed fissures at the 6 and 12 o’clock positions, associated with a sentinel tag and a hypertonic anal sphincter.
The patient underwent Ksharakarma, a para-surgical Ayurvedic procedure, along with excision of the sentinel tag under local anaesthesia. Post-procedure management included Ayurvedic internal medications, regular wound dressing, and dietary regulation.
At the time of discharge, the patient reported significant relief from pain, with normal bowel function and absence of bleeding. She was advised adequate rest, follow-up wound care, and adherence to a light pathya diet to promote optimal healing.
“I had recurrent anal fistula and even underwent three surgeries, but the problem kept coming back.
I turned to Apollo AyurVAID and consulted Dr. Kalpita Thakre, who listened
carefully to my history and conducted thorough scans. After her Ayurvedic treatment, my condition improved
drastically—I can now sit, walk, and sleep comfortably, and feel confident that there will be no recurrence.
I am truly grateful for the skill and compassionate care at Apollo AyurVAID, and highly recommend them to
anyone with similar issues.”
Mr. PG, 35 years
As we work hard to improve our services, your feedback is important to us. Please take a moment to help us serve you better.
The information provided in this blog is for general informational purposes only and is not intended as a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician, Ayurvedic practitioner, or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment.
Subscribe to our hospital newsletter for the latest health tips, updates on services, patient stories, and community events. Sign up today and stay informed!





Popular Searches: DiseasesTreatmentsDoctorsHospitalsWhole person careRefer a patientInsurance